Introduction
Medical research has witnessed remarkable advancements with gene editing, particularly through the CRISPR-Cas9 system. However, there’s another powerful player in the field – human-induced pluripotent stem cells (hiPSCs). Together, these two revolutionary tools are reshaping our understanding of human diseases and opening doors to novel therapeutic strategies.
The potential of hiPSCs
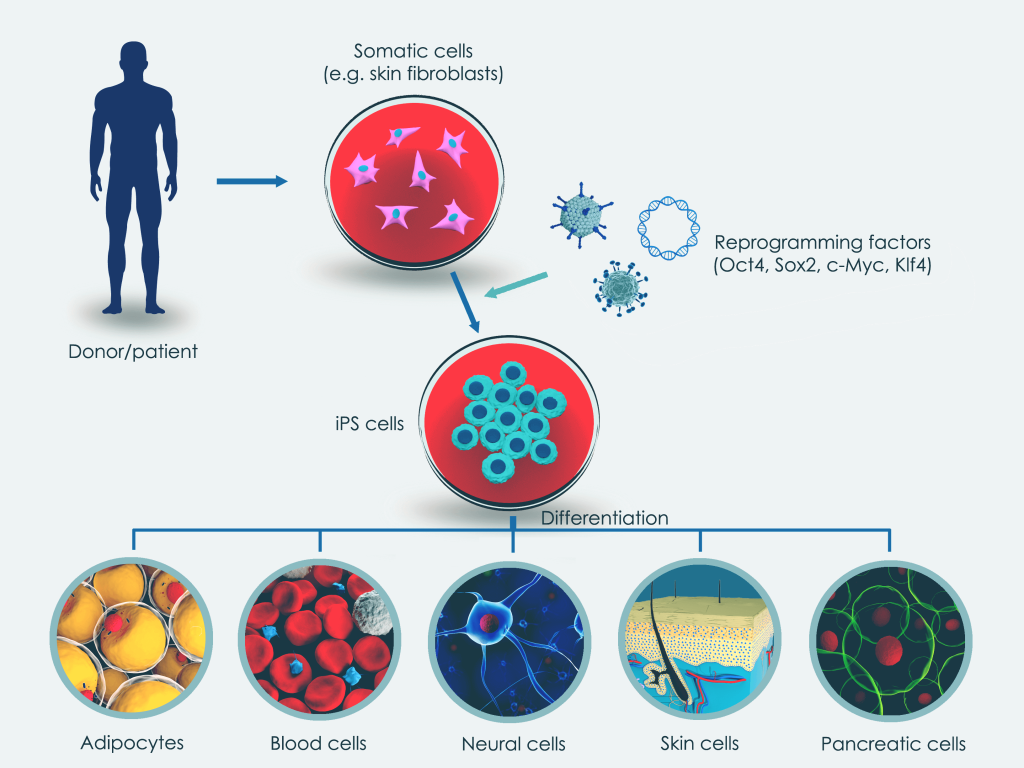
hiPSCs are self-renewing cells capable of differentiating into any cell type, making them a versatile tool in medicine, molecular biology, and genetics. Obtained through the direct reprogramming of somatic cells, hiPSCs offer unique opportunities to model diseases, discover drugs, and develop effective therapies.
From somatic cells to sophisticated patient-centric cell models
Somatic cells are collected from donors or patients via blood samples or skin biopsies. These cells are then reprogrammed using specific transcription factors, inducing pluripotency in the hiPSCs. The resulting hiPSCs can be directed to differentiate into various cell types for disease modelling, drug discovery, and tissue engineering.
- Somatic cells are obtained from a healthy donor or patient via a blood sample or a skin biopsy.
- The somatic cells are reprogrammed through gene transfer of distinct transcription factors (‘reprogramming factors’) that induce pluripotency.
- The resulting hiPSCs can then be instructed to differentiate into, for example, muscle cells or neuronal cells that can be used for applications such as disease modelling, drug discovery and tissue engineering.
Beyond their therapeutic promise, hiPSCs replace the need for embryonic stem cells in research, avoiding ethical controversies associated with the destruction of human embryos.
Gene-editing hiPSCs with CRISPR-Cas9
Combining CRISPR-Cas9 with hiPSCs allows for fast, cost-effective, and precise genetic modifications. This combination facilitates the investigation of diseases in a patient-specific genetic context, advancing its translation into real-life applications. Gene-edited hiPSCs allow for the creation of isogenic pairs of cells, invaluable for studying disease characteristics and identifying causative mutations and underlying mechanisms. This approach is particularly useful in disease research. Additionally, hiPSCs and CRISPR-Cas9 play a role in gene therapy, potentially correcting disease-causing mutations like beta-thalassemia.
Challenges
Despite the promising potential of utilizing gene-edited and tailored hiPSCs for disease modelling and research, challenges remain. The successful generation of gene-edited hiPSCs requires a carefully designed strategy and appropriate gene-editing reagents. For example, guide RNAs and repair templates need to be efficient while minimizing potential off-target effects. Aside, as hiPSCs are sensitive to changes in their environment, gentle handling and appropriate manipulation techniques are critical to obtain high-quality cell models.
At iotaSciences, we offer expert CRISPR-Cas9 services for hiPSCs to accelerate your research. Enquire about our offerings today!